The stroke volume calculator helps you determine the amount of blood pumped by the left ventricle in one contraction. Understanding how to calculate stroke volume is fundamental, as it’s a key component of cardiac output. This page provides methods for echo stroke volume calculation (using LVOT VTI) and the classic End-Diastolic Volume (EDV) minus End-Systolic Volume (ESV) method.
What is Stroke Volume?
Stroke Volume (SV) is the volume of blood ejected from a ventricle (typically the left ventricle) during one heartbeat (systole). It is usually measured in milliliters (mL) per beat. SV is a crucial indicator of cardiac contractile function and overall cardiovascular health.
Stroke volume, along with heart rate, determines cardiac output (CO = SV × HR). You can learn more about this relationship in our article What is Cardiac Output?.
Stroke Volume Calculation Methods
There are several ways to calculate or estimate stroke volume:
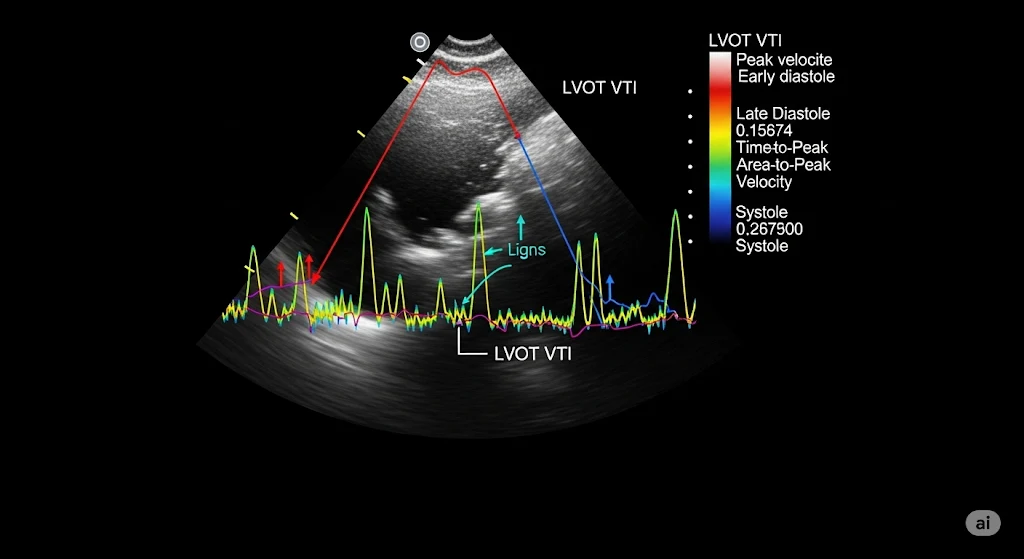
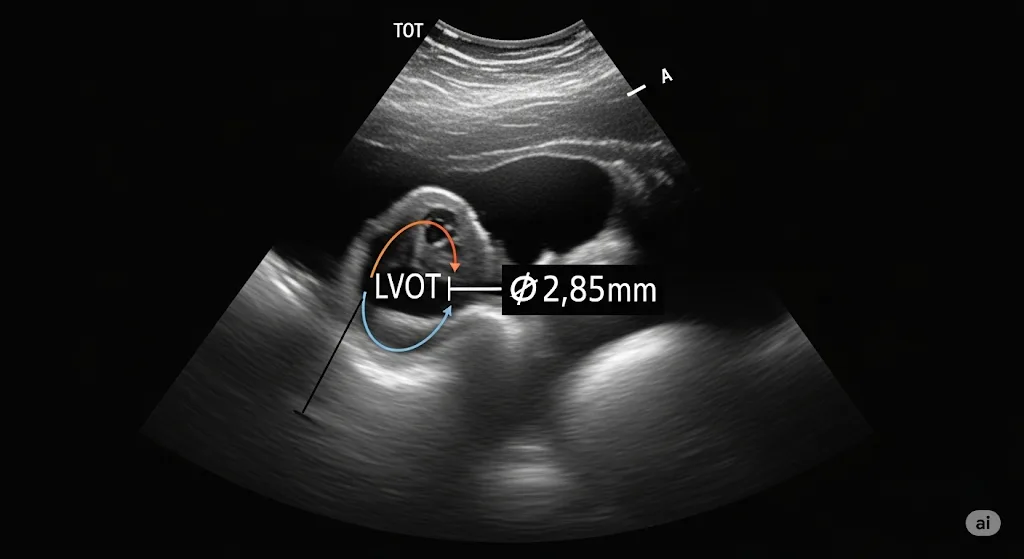
1. Echocardiography (Doppler Method – LVOT VTI)
This is a common non-invasive method using Doppler ultrasound. Our Doppler Echo Cardiac Output Calculator uses this principle.
Formula: SV (mL) = LVOT CSA (cm2) × LVOT VTI (cm)
- LVOT CSA (Left Ventricular Outflow Tract Cross-Sectional Area): Calculated from the LVOT diameter (D) as CSA = π × (D/2)2. The diameter is measured in the parasternal long-axis view.
- LVOT VTI (Velocity Time Integral): Measured using pulsed-wave Doppler in the LVOT from an apical view. It represents the distance blood travels through the LVOT with each beat.
Stroke Volume Calculator (LVOT VTI Method)
Results:
LVOT CSA: – cm²
Stroke Volume (SV): – mL
Formulas:
LVOT CSA = π × (LVOT Diameter/2)²
SV (mL) = LVOT CSA × VTI
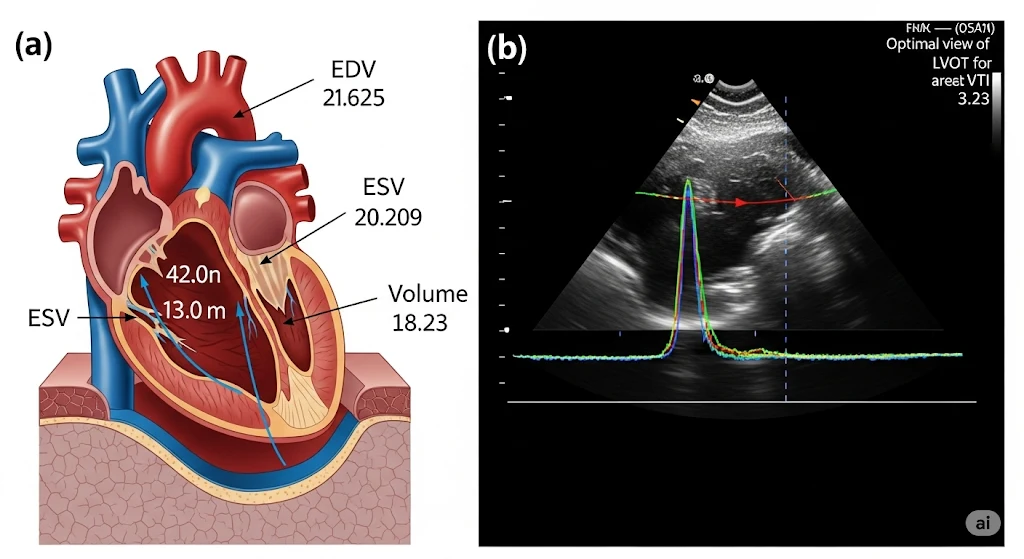
2. Volumetric Method (EDV - ESV)
This method relies on measuring ventricular volumes at the end of diastole (EDV - maximum filling) and the end of systole (ESV - minimum volume after contraction).
Formula: SV (mL) = EDV (mL) - ESV (mL)
- End-Diastolic Volume (EDV): The volume of blood in the ventricle just before contraction.
- End-Systolic Volume (ESV): The volume of blood remaining in the ventricle immediately after contraction.
These volumes can be estimated using echocardiography (e.g., Simpson's biplane method), cardiac MRI (considered a gold standard for volumes), or radionuclide ventriculography.
Stroke Volume Calculator (EDV-ESV Method)
Results:
Stroke Volume (SV): - mL
Ejection Fraction (EF): - %
Formulas:
SV (mL) = EDV - ESV
EF (%) = (SV / EDV) × 100
This method also allows for the calculation of Ejection Fraction (EF) = (SV / EDV) × 100%, a key indicator of systolic function.
Normal Stroke Volume Values
Normal stroke volume in a resting healthy adult is typically between 60 mL and 100 mL. However, this can vary based on factors like age, sex, body size, and fitness level. Athletes often have larger stroke volumes. For specific population values, it's best to consult clinical guidelines and resources like the American Society of Echocardiography guidelines.
To see how SV contributes to overall cardiac function, check our general Cardiac Output Calculator dashboard.
Factors Affecting Stroke Volume
Three main factors influence stroke volume, as detailed in our article on factors influencing cardiac output:
- Preload: The stretch on the ventricular muscle fibers before contraction (related to EDV). Increased preload (within physiological limits) generally increases SV (Frank-Starling mechanism).
- Afterload: The resistance the ventricle must overcome to eject blood. Increased afterload (e.g., high blood pressure, aortic stenosis) generally decreases SV.
- Contractility (Inotropy): The inherent strength of ventricular contraction, independent of preload and afterload. Increased contractility increases SV.
Clinical Significance of Stroke Volume
Assessing stroke volume is important for:
- Diagnosing and managing heart failure, where SV is often reduced. More on CO in heart failure.
- Evaluating valvular heart disease (e.g., aortic regurgitation can increase total SV, while aortic stenosis can decrease effective SV).
- Monitoring patients in critical care, guiding fluid therapy and inotropic support. The clinical significance of CO and its components is vast.
- Assessing response to cardiovascular medications.
- Understanding athletic performance and cardiac adaptation.
Stroke volume can also be indexed to body surface area (BSA) to get Stroke Volume Index (SVI), similar to how Cardiac Index is derived from CO.
Linking Stroke Volume to Cardiac Output
Once you have calculated Stroke Volume (SV) and know the Heart Rate (HR), you can easily calculate Cardiac Output (CO):
![]()
For further information on cardiovascular physiology, resources from the National Heart, Lung, and Blood Institute (NHLBI) are highly recommended.