Understanding what cardiac output is forms the bedrock of assessing cardiovascular health and function. Simply put, cardiac output (often abbreviated as CO or Q) is the volume of blood pumped by the heart – specifically by the left or right ventricle – per minute. It’s a critical measure of how effectively your heart is working to supply oxygen and nutrients to the rest of your body. This article will break down the cardiac output definition, explain its importance, and touch upon normal ranges.
Defining Cardiac Output: The Core Formula
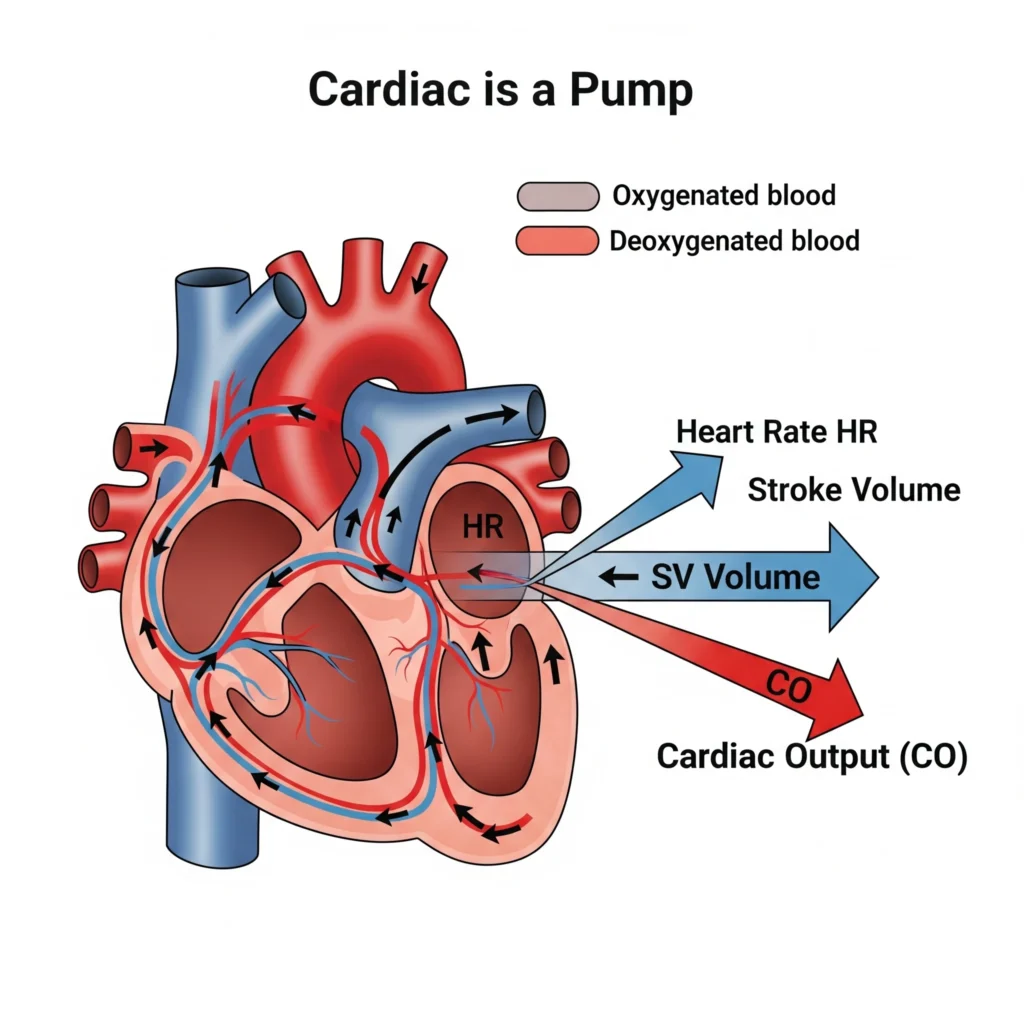
The fundamental formula to understand and calculate cardiac output is:
Cardiac Output (CO) = Heart Rate (HR) × Stroke Volume (SV)
Let’s break down these components:
- Heart Rate (HR): This is the number of times your heart beats per minute (bpm). It’s easily measurable by taking your pulse.
- Stroke Volume (SV): This is the volume of blood pumped from one ventricle (usually the left ventricle is referred to) with each heartbeat, typically measured in milliliters per beat (mL/beat). You can use our stroke volume calculator for this.
For example, if an individual has a heart rate of 70 bpm and a stroke volume of 70 mL/beat, their cardiac output would be 4900 mL/minute, or 4.9 L/minute.
Why is Cardiac Output Important?
Cardiac output is a vital physiological parameter for several reasons:
- Oxygen and Nutrient Delivery: The primary role of CO is to ensure adequate delivery of oxygenated blood and nutrients to all tissues and organs in the body. Insufficient CO can lead to organ dysfunction.
- Waste Removal: Efficient CO also facilitates the removal of metabolic waste products (like carbon dioxide) from tissues.
- Indicator of Heart Health: CO directly reflects the heart’s pumping ability. A significantly low or abnormally high CO can indicate underlying cardiac conditions such as heart failure, valvular disease, or shock. The impact of various medical conditions on CO is significant.
- Guiding Medical Treatment: In clinical settings, especially critical care, monitoring cardiac output helps doctors assess a patient’s hemodynamic status and guide treatment decisions, such as fluid administration or medication adjustments.
- Response to Physiological Demands: CO isn’t static; it changes based on the body’s needs. During exercise, for instance, CO increases to meet the higher oxygen demand of muscles. Understanding these factors affecting cardiac output is crucial.
Normal Cardiac Output Ranges
In a healthy resting adult, normal cardiac output is typically between 4.0 to 8.0 liters per minute (L/min). However, this range can vary based on several factors:
- Age: CO may change with age. Pediatric cardiac output, for example, is scaled to body size.
- Body Size: Larger individuals generally have a higher CO. To account for this, cardiac output is often indexed to body surface area (BSA), resulting in the Cardiac Index (CI). You can use our cardiac index calculator for this.
- Fitness Level: Athletes often have a higher stroke volume and thus can achieve a higher maximum CO during exertion, and sometimes a lower resting heart rate.
- Metabolic State: Conditions like fever or hyperthyroidism can increase CO, while hypothermia can decrease it.
For a detailed breakdown, please see our page on normal cardiac output values.
Frequently Asked Questions (FAQ) about Cardiac Output
What happens if cardiac output is too low?
If cardiac output is too low, tissues and organs may not receive enough oxygen and nutrients (a state called hypoperfusion). This can lead to symptoms like fatigue, dizziness, organ damage, and in severe cases, shock. Conditions like heart failure often result in low cardiac output.
What happens if cardiac output is too high?
Persistently high cardiac output can also be problematic, potentially indicating conditions like severe anemia, sepsis, hyperthyroidism, or arteriovenous fistulas. While the heart is working harder, it may not always be efficient or sustainable. It’s important to investigate the underlying cause. You can explore some of these scenarios in our cardiac output case studies.
How is cardiac output measured?
Cardiac output can be measured or estimated using various methods, ranging from invasive techniques like thermodilution (often requiring a pulmonary artery catheter) or the Fick method, to non-invasive methods like echocardiography (Doppler). Our main calculator page links to tools for these methods.
Understanding cardiac output is fundamental to appreciating the marvel of the human circulatory system. For more detailed information, consult resources like the National Heart, Lung, and Blood Institute (NHLBI) or the Circulation journal by the AHA for advanced research.
Explore our range of calculators to delve deeper into specific measurement techniques.