Cardiac output (CO), the amount of blood pumped by the heart per minute, is a dynamic physiological parameter influenced by several key factors. Understanding these factors affecting cardiac output is crucial for grasping cardiovascular physiology and interpreting changes in CO. The four primary determinants are preload, afterload, myocardial contractility, and heart rate. This article delves into each, explaining their impact, including what constitutes an increase in cardiac afterload and generally, what increases afterload.
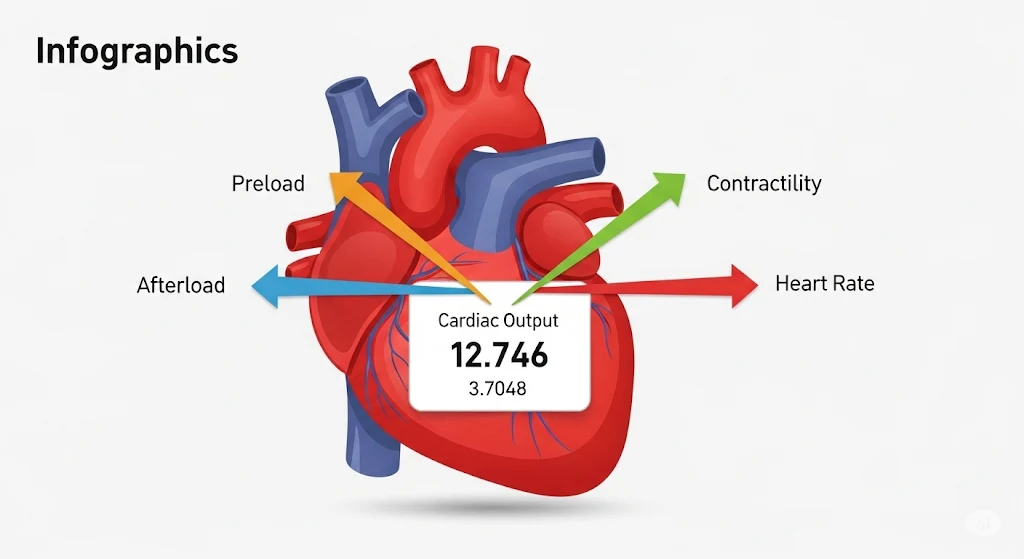
Recall: Cardiac Output = Heart Rate × Stroke Volume
Before diving into the factors, remember the basic formula from our “What is Cardiac Output?” article: CO = HR × SV.
Heart rate is one direct factor. The other three factors (preload, afterload, contractility) primarily influence Stroke Volume (SV), which is the volume of blood pumped per beat. You can calculate SV with our Stroke Volume Calculator.
1. Preload
Definition: Preload is the degree of stretch on the ventricular muscle fibers at the end of diastole (just before contraction). It’s essentially the “load” or volume of blood that fills the ventricle during diastole, determining the initial muscle fiber length.
Clinical Correlate: Often related to End-Diastolic Volume (EDV) or End-Diastolic Pressure (EDP). Central Venous Pressure (CVP) can be a surrogate for right ventricular preload, and Pulmonary Capillary Wedge Pressure (PCWP) for left ventricular preload.
Impact on CO:
According to the Frank-Starling mechanism, an increase in preload (i.e., more ventricular filling) leads to a more forceful contraction and thus an increased stroke volume, up to a physiological limit. Beyond this limit, overstretching can decrease contractility.
Factors Increasing Preload:
- Increased venous return (e.g., fluid administration, leg raises)
- Slower heart rate (allows more time for ventricular filling)
- Increased ventricular compliance
- Conditions like mitral regurgitation or aortic regurgitation (volume overload)
Factors Decreasing Preload:
- Decreased venous return (e.g., hemorrhage, dehydration, venodilators like nitroglycerin)
- Rapid heart rate (less filling time)
- Decreased ventricular compliance (e.g., hypertrophy, pericardial effusion)
(Conceptual Interactive Element: A slider or animation showing how increasing preload stretches the ventricle and (initially) increases stroke volume on a Frank-Starling curve.)
2. Afterload
Definition: Afterload is the resistance or pressure the ventricle must overcome to eject blood into the aorta (for the left ventricle) or pulmonary artery (for the right ventricle) during systole. It’s the “load” the heart pumps against.
Clinical Correlate: For the left ventricle, afterload is closely related to Systemic Vascular Resistance (SVR) and aortic pressure. For the right ventricle, it’s related to Pulmonary Vascular Resistance (PVR) and pulmonary artery pressure.
Impact on CO:
An increase in cardiac afterload makes it harder for the ventricle to eject blood, leading to a decrease in stroke volume (assuming contractility and preload remain constant). Conversely, a decrease in afterload allows the ventricle to eject more blood, increasing SV.
What Increases Afterload (Factors Increasing Afterload)?
- Systemic Hypertension: High blood pressure directly increases the resistance the LV must pump against.
- Aortic Stenosis: Narrowing of the aortic valve creates a significant obstruction to LV outflow.
- Vasoconstriction: Systemic vasoconstrictors (e.g., phenylephrine, high doses of norepinephrine) increase SVR.
- Increased blood viscosity
- For the RV: Pulmonary hypertension, pulmonary embolism, pulmonic stenosis.
Factors Decreasing Afterload:
- Vasodilators (e.g., ACE inhibitors, nitrates, calcium channel blockers) reduce SVR.
- Decreased blood pressure (hypotension).
- For the RV: Pulmonary vasodilators.
(Conceptual Interactive Element: A visual of the ventricle pumping against a variable resistance (e.g., a narrowing pipe), showing SV decreasing as resistance increases.)
3. Myocardial Contractility (Inotropy)
Definition: Contractility refers to the intrinsic ability of the heart muscle (myocardium) to contract and generate force, independent of changes in preload or afterload. It reflects the efficiency of the heart’s pumping action.
Impact on CO:
Increased contractility leads to a more forceful contraction, ejecting a larger stroke volume for any given preload and afterload. Decreased contractility weakens the contraction, reducing stroke volume.
Factors Increasing Contractility (Positive Inotropes):
- Sympathetic nervous system stimulation (e.g., release of norepinephrine, epinephrine)
- Inotropic drugs (e.g., dopamine, dobutamine, digoxin, milrinone)
- Increased intracellular calcium levels
- Increased heart rate (Bowditch effect/treppe phenomenon, to a certain extent)
Factors Decreasing Contractility (Negative Inotropes):
- Parasympathetic nervous system stimulation (primarily affects atria)
- Myocardial ischemia or infarction (heart attack)
- Cardiomyopathy
- Hypoxia, acidosis
- Certain drugs (e.g., beta-blockers, calcium channel blockers – though their effect on CO is complex and often beneficial by reducing HR and afterload in some contexts)
(Conceptual Interactive Element: An animation of heart muscle fibers contracting with varying force, linked to changes in SV.)
4. Heart Rate (Chronotropy)
Definition: Heart rate is the number of times the heart beats per minute (bpm).
Impact on CO:
An increase in heart rate generally increases cardiac output, provided stroke volume is maintained. However, at very high heart rates, diastolic filling time is significantly reduced. This can decrease preload and thus stroke volume, potentially leading to a decrease in cardiac output despite the fast rate.
Factors Increasing Heart Rate (Positive Chronotropes):
- Sympathetic stimulation
- Drugs like atropine, epinephrine, isoproterenol
- Fever, hyperthyroidism, anxiety, exercise
Factors Decreasing Heart Rate (Negative Chronotropes):
- Parasympathetic (vagal) stimulation
- Drugs like beta-blockers, some calcium channel blockers, digoxin (at toxic levels)
- Hypothyroidism, athletic conditioning (at rest)
(Conceptual Interactive Element: A graph showing CO increasing with HR up to an optimal point, then potentially decreasing at very high rates due to reduced filling time.)
Interplay of Factors
It’s important to remember that these four factors are often interrelated and can influence each other. For example, a drug that increases contractility might also affect heart rate or vascular resistance (afterload). The body has complex regulatory mechanisms (like the baroreceptor reflex) to maintain adequate cardiac output and blood pressure. Many medical conditions affect these factors.
Understanding these determinants is crucial for interpreting measurements from our cardiac output calculator and for understanding various cardiovascular diseases and their treatments. For more in-depth physiology, consult resources like Guyton and Hall Textbook of Medical Physiology or AHA’s Circulation: Arrhythmia and Electrophysiology journal.
Explore how these factors are relevant in clinical scenarios involving cardiac output monitoring.