In cardiovascular medicine, both Cardiac Output (CO) and Cardiac Index (CI) are vital measures of heart performance. While related, they offer different perspectives. This article clarifies the distinction between cardiac output vs cardiac index, explains their respective clinical use-cases, and provides a comparative chart to highlight their differences. Understanding this is crucial before using tools like our main cardiac output calculator or the specific Cardiac Index Calculator.
Defining Cardiac Output (CO)
Cardiac Output (CO) is the total volume of blood pumped by the heart’s ventricle (typically the left ventricle) in one minute. It’s a fundamental measure of the heart’s ability to supply blood to the body.
Formula: CO = Heart Rate (HR) × Stroke Volume (SV)
Units: Liters per minute (L/min)
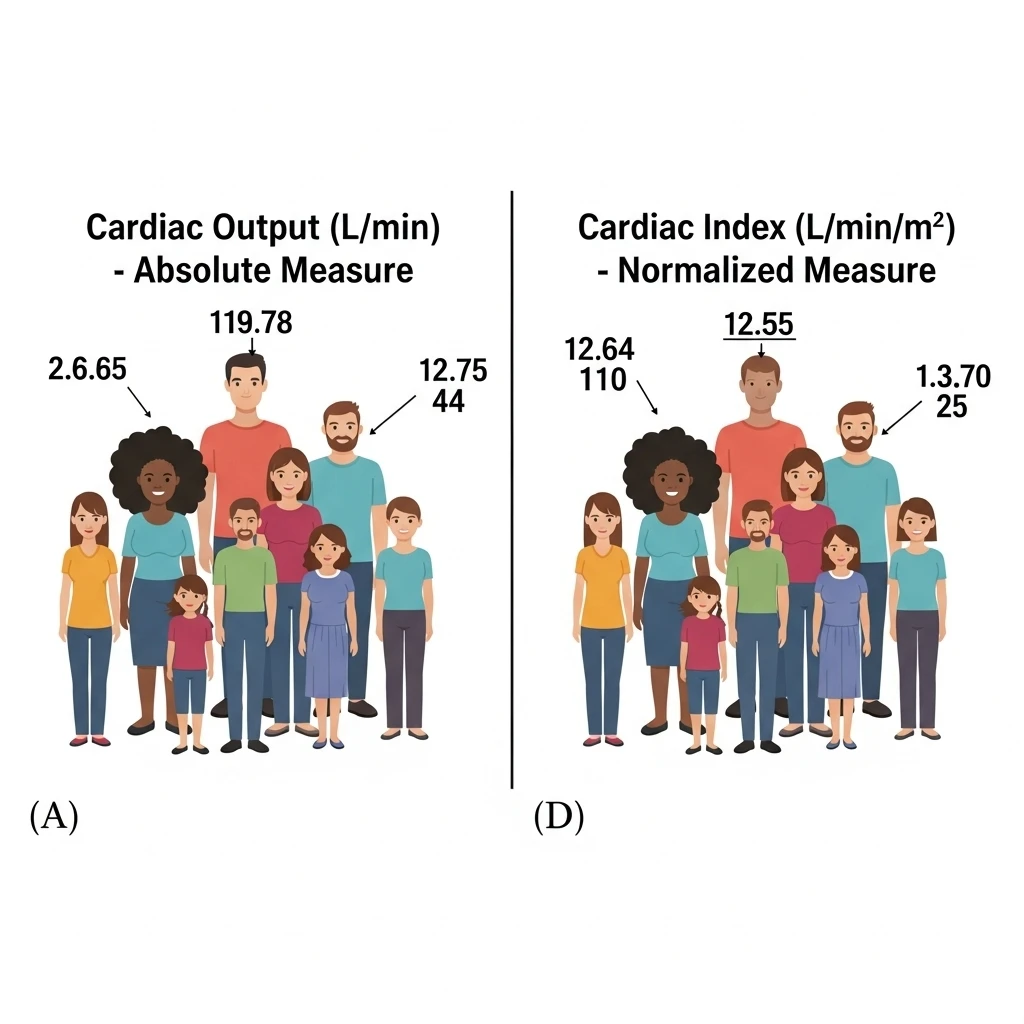
CO is an absolute measure. For example, a CO of 5 L/min means the heart pumps 5 liters of blood each minute. You can learn more about its basics in “What is Cardiac Output?”.
Defining Cardiac Index (CI)
Cardiac Index (CI) is cardiac output adjusted for an individual’s body size, specifically their Body Surface Area (BSA). It provides a more standardized measure of heart performance, allowing for more meaningful comparisons between individuals of different sizes.
Formula: CI = Cardiac Output (CO) / Body Surface Area (BSA)
Units: Liters per minute per square meter (L/min/m2)
CI normalizes CO, making it a relative measure. A CI of 3.0 L/min/m2 means the heart pumps 3 liters of blood per minute for every square meter of the person’s body surface area.
Key Differences: Cardiac Output vs. Cardiac Index
| Feature | Cardiac Output (CO) | Cardiac Index (CI) |
|---|---|---|
| Definition | Total blood volume pumped per minute | CO normalized to body surface area |
| Nature of Measure | Absolute | Relative (indexed to body size) |
| Units | L/min | L/min/m2 |
| Primary Use | Overall measure of heart pump function | Comparing heart function between individuals of different sizes; more precise assessment of tissue perfusion adequacy relative to metabolic need. |
| Dependency on Body Size | Highly dependent (larger individuals generally have higher CO) | Less dependent (corrects for body size) |
| Normal Range (Adult at Rest) | ~4.0 – 8.0 L/min (varies with size) | ~2.5 – 4.0 L/min/m2 (more consistent across sizes) |
For a list of normal values, see our normal cardiac output values page.
Clinical Use-Cases and Scenarios
When is Cardiac Output (CO) primarily used?
- General Assessment: Provides a quick overview of the heart’s pumping capacity.
- Tracking Individual Changes: Useful for monitoring changes in an individual patient over time, assuming their body size remains relatively constant.
- Basic Physiological Understanding: Essential for understanding the core function of the heart. You can explore how CO is calculated through various methods.
When is Cardiac Index (CI) preferred?
- Comparing Different Patients: Essential when comparing the cardiac function of individuals with significantly different body sizes (e.g., a small child vs. a large adult). This is particularly relevant for pediatric cardiac output.
- Critical Care Settings (ICU): CI is a standard parameter for assessing hemodynamic status and guiding therapy (fluids, inotropes) because it better reflects the adequacy of perfusion relative to metabolic demands. It helps in understanding clinical significance in critical states.
- Heart Failure Management: CI provides a more accurate measure of pump dysfunction severity and response to therapy across diverse patient populations. Changes in CO are often seen in various medical conditions like heart failure or sepsis.
- Research Studies: When studying cardiac function across populations, CI allows for standardized comparisons.
- Prognostication: CI often has stronger prognostic value than CO alone in many critical illnesses.
Example Scenario: Shock
Consider two patients in shock:
- Patient A (Large Adult, BSA 2.2 m2): CO = 4.4 L/min. This might seem borderline low.
CI = 4.4 L/min / 2.2 m2 = 2.0 L/min/m2. This CI is clearly low, indicating significant hypoperfusion relative to body size. - Patient B (Small Adult, BSA 1.5 m2): CO = 3.3 L/min. This CO appears quite low.
CI = 3.3 L/min / 1.5 m2 = 2.2 L/min/m2. This CI is also low, but perhaps less severely depressed relative to their size than Patient A’s CO might initially suggest without indexing.
In both cases, CI provides a more nuanced understanding of the severity of cardiogenic shock relative to the patient’s individual needs.
Conclusion: CO and CI are Complementary
Cardiac Output and Cardiac Index are not mutually exclusive; they are complementary measures. CO tells us the raw amount of blood being pumped, while CI refines this by considering the patient’s body size, offering a more standardized and often more clinically relevant assessment of cardiac performance, especially in diverse populations or critical care.
Understanding this distinction is vital for accurate interpretation of hemodynamic data. For further insights into factors that can alter these values, read about factors affecting cardiac output.
For more in-depth physiological information, consult resources like the American Physiological Society or major cardiology journals like the Journal of the American College of Cardiology.
Ready to calculate? Visit our calculators hub for tools to measure both CO and CI.