Our Cardiac Index (CI) Calculator helps you assess heart performance relative to body size by normalizing cardiac output (CO) to Body Surface Area (BSA). This page explains the cardiac index formula, how to use the calculator (which includes an integrated BSA calculator), discusses the normal cardiac index range, and its clinical importance. Understanding the difference between cardiac output vs cardiac index is key for proper interpretation.
Cardiac Index Calculator (with BSA Calculation)
Results:
Cardiac Index (CI): – L/min/m²
- Normal: 2.5-4.0 L/min/m²
- Low: <2.5 L/min/m²
- High: >4.0 L/min/m²
Cardiac Index Formula:
CI = CO / BSA
Where:
- CI = Cardiac Index (L/min/m²)
- CO = Cardiac Output (L/min)
- BSA = Body Surface Area (m²)
What is Cardiac Index?
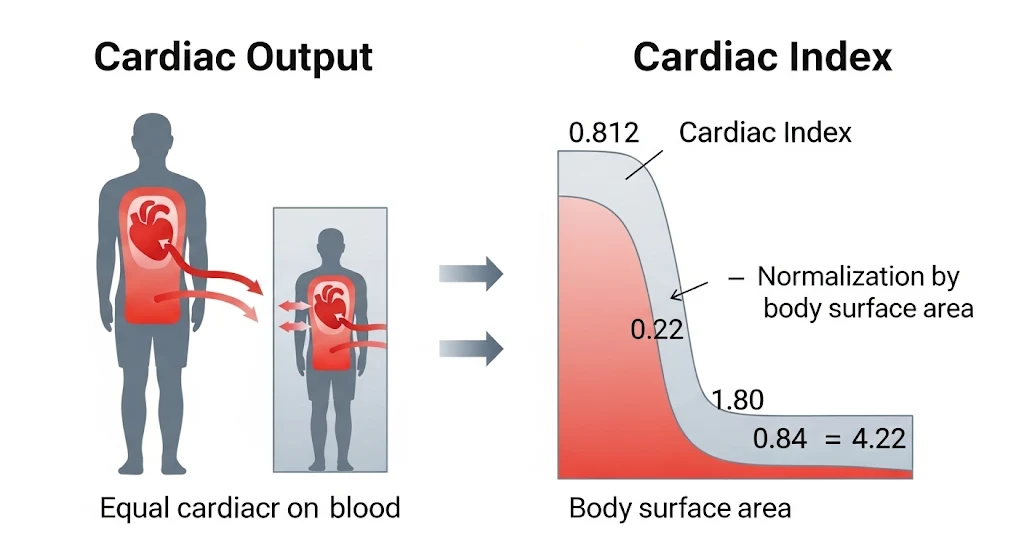
Cardiac Index (CI) is a hemodynamic parameter that relates the cardiac output (CO) from the left ventricle in one minute to the body surface area (BSA). By doing so, it provides a more comparable measure of heart pump performance across individuals of varying sizes. While cardiac output is an absolute measure, cardiac index offers a relative assessment.
Formula:
![]()
Normal Cardiac Index Range
The generally accepted normal cardiac index range for adults at rest is 2.5 to 4.0 L/min/m2. Values may vary slightly based on age and specific clinical context. Referencing normal values for cardiac output and index is always important.
- Low Cardiac Index (<2.5 L/min/m2): May indicate hypoperfusion or impaired cardiac function relative to body size. This could be due to conditions like heart failure, shock (cardiogenic, hypovolemic), or severe valvular disease. This is a common finding in patients with decreased cardiac output conditions.
- High Cardiac Index (>4.0 L/min/m2): May indicate a hyperdynamic state, seen in conditions like sepsis (early stages), severe anemia, hyperthyroidism, pregnancy, or arteriovenous fistulas.
Clinical Significance and Interpretation
Cardiac Index is a more precise indicator of circulatory adequacy than CO alone, especially when comparing patients of different sizes or tracking an individual patient whose weight might change significantly (e.g., due to fluid shifts).
- Critical Care: CI is extensively used in ICUs to guide therapy for shock, heart failure, and post-operative cardiac patients. It helps in decisions about fluid administration, vasopressors, and inotropes. The clinical use of CO monitoring often involves CI.
- Heart Failure Management: CI helps classify heart failure severity and monitor response to treatment.
- Prognostication: A low CI is often associated with poorer outcomes in various critical illnesses.
- Pediatrics: CI is particularly important in pediatric cardiology due to rapid changes in body size with growth.
Explaining Hypoperfusion and High-Output States
Hypoperfusion (Low CI): When the CI is low, it suggests that the heart is not pumping enough blood to meet the metabolic demands of the body's tissues, adjusted for body size. This can lead to symptoms like cool extremities, altered mental status, decreased urine output, and eventually organ dysfunction if not corrected.
High-Output States (High CI): A high CI indicates that the heart is pumping an unusually large volume of blood relative to body size. While this might seem good, it can be a sign of an underlying problem (like sepsis where vasodilation reduces systemic vascular resistance) or put undue strain on the heart over time.
Relationship with Other Hemodynamic Parameters
Cardiac Index is often considered alongside other parameters like:
- Mean Arterial Pressure (MAP): To assess tissue perfusion pressure.
- Systemic Vascular Resistance Index (SVRI): SVRI = (MAP - CVP) / CI × 80. This helps differentiate causes of low CI (e.g., low CI with high SVRI in cardiogenic shock vs. low CI with low SVRI in distributive shock).
- Stroke Volume Index (SVI): SVI = SV / BSA. CI = SVI × HR. Our Stroke Volume Calculator can help determine SV.
For more information on hemodynamic monitoring in critical care, resources like the European Society of Intensive Care Medicine (ESICM) provide valuable guidelines and research.
Remember, the interpretation of CI should always be in the context of the overall clinical picture, including other vital signs, patient history, and current therapies. Explore our blog for more in-depth articles on cardiac physiology.