Our Doppler echo cardiac output calculator provides a non-invasive method to estimate cardiac output (CO) using common echocardiographic measurements. This technique is widely used due to its accessibility and ability to provide real-time hemodynamic data. This page explains how to use the calculator, the principles behind cardiac output echo calculations, and the importance of measurements like LVOT VTI (Left Ventricular Outflow Tract Velocity Time Integral).
Doppler Echo Cardiac Output Calculator
Results:
Stroke Volume (SV): – mL
Cardiac Output (CO): – L/min
Cardiac Index (CI): – L/min/m²
Calculation Formulas:
LVOT Area = π × (LVOT Diameter/2)²
Stroke Volume (SV) = LVOT Area × VTI
Cardiac Output (CO) = SV × HR / 1000
Cardiac Index (CI) = CO / BSA (using standard 1.73 m²)
Where:
- VTI = Velocity Time Integral (cm)
- LVOT = Left Ventricular Outflow Tract
- HR = Heart Rate (beats per minute)
- BSA = Body Surface Area
Principle of Doppler Echocardiography for Cardiac Output
The calculation of cardiac output by Doppler echocardiography is based on the principle that flow (Q) through a cylindrical structure is the product of its cross-sectional area (CSA) and the mean velocity of blood flow over time (Velocity Time Integral, VTI).
Specifically for cardiac output via the LVOT:
- Stroke Volume (SV) Calculation:
- The LVOT is assumed to be roughly circular. Its diameter (DLVOT) is measured to calculate the CSALVOT = π × (DLVOT / 2)2.
- The VTILVOT is measured using pulsed-wave Doppler across the LVOT. This represents the distance a column of blood travels with each heartbeat.
- Stroke Volume (SV) = CSALVOT × VTILVOT. You can also use our dedicated stroke volume calculator.
- Cardiac Output (CO) Calculation:
- Heart Rate (HR) is obtained (e.g., from EKG during the echo).
- Cardiac Output (CO) = SV × HR.
Understanding what cardiac output is fundamentally helps in appreciating this non-invasive measurement technique.
How to Obtain Measurements for the Calculator
Step-by-Step Guide:
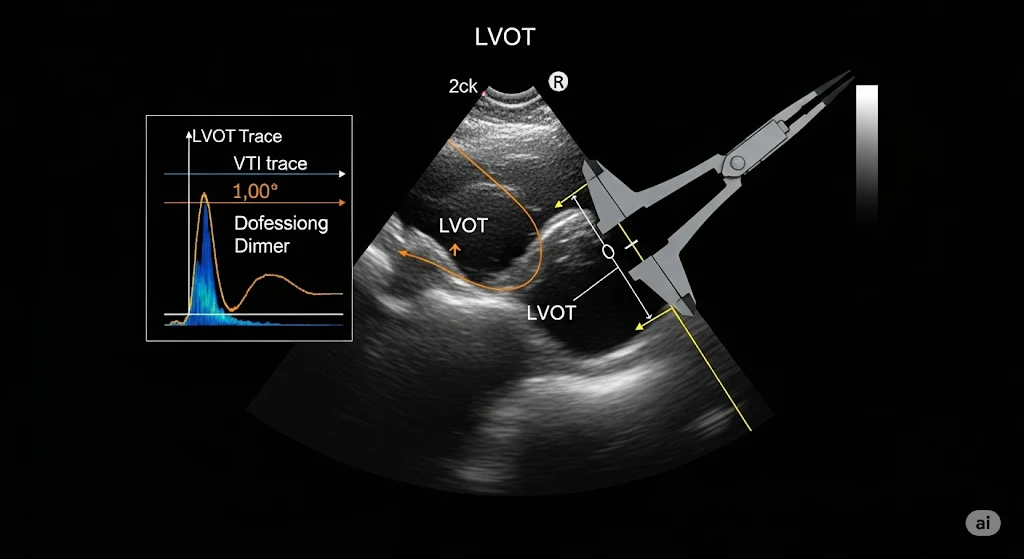
- Measure LVOT Diameter (DLVOT):
- Typically measured in the parasternal long-axis (PLAX) view.
- Measure from inner-edge to inner-edge at the level of the aortic valve annulus (where the leaflets insert) during mid-systole.
- Accuracy is crucial as this value is squared in the CSA calculation, magnifying errors. The American Society of Echocardiography provides guidelines on these measurements.
- Commonly around 1.8 – 2.4 cm in adults.
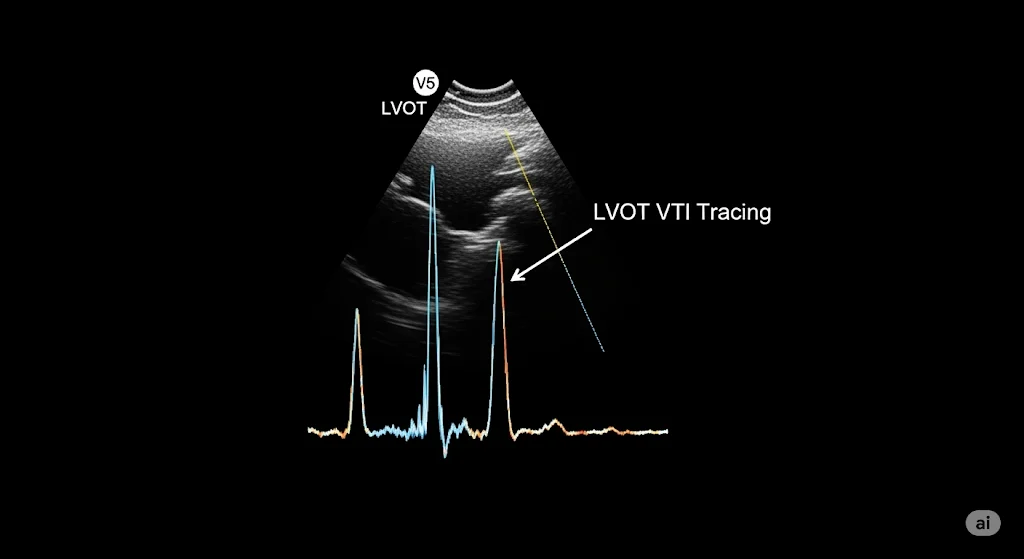
2. Measure LVOT Velocity Time Integral (VTILVOT):
- Typically measured using pulsed-wave (PW) Doppler.
- Place the sample volume in the LVOT, just proximal to the aortic valve, from an apical 5-chamber or apical 3-chamber view.
- Ensure a clean spectral Doppler envelope with minimal spectral broadening.
- Trace the modal velocity (outer edge) of the systolic flow profile. The machine calculates the VTI.
- Average of 3-5 beats is recommended, more if arrhythmia is present.
- Commonly around 18-25 cm in adults.
3. Determine Heart Rate (HR):
- Usually recorded automatically by the echocardiography machine from the EKG during the acquisition of VTI.
4. Input Values into the Calculator: Use the measured values.
Clinical Applications and Utility
Doppler-derived CO is widely used due to its non-invasive nature:
- Routine Echocardiography: Part of a comprehensive hemodynamic assessment.
- Heart Failure Management: To assess and monitor LV systolic function and response to therapy. Understanding CO in heart failure is vital.
- Critical Care: For quick, non-invasive CO estimation in hemodynamically unstable patients, though it may be less accurate than invasive methods in complex cases. See a comparison with the Fick method.
- Valvular Heart Disease: To assess the hemodynamic significance of valvular lesions.
- Perioperative Setting: For guiding fluid management and assessing cardiac function.
Advantages and Limitations
Advantages:
- Non-invasive: Safe and repeatable.
- Readily Available: Echocardiography machines are common in most healthcare settings.
- Provides Additional Information: A full echo exam yields much more data about cardiac structure and function.
Limitations:
- Operator Dependent: Accuracy heavily relies on sonographer skill and experience.
- Acoustic Window: Poor image quality can hinder accurate measurements.
- Geometric Assumptions: Assumes circular LVOT; variations can lead to errors. LVOT diameter measurement error is magnified.
- Arrhythmias: Beat-to-beat variability (e.g., in atrial fibrillation) can make averaging VTI challenging.
- Aortic Stenosis/Regurgitation: Can affect accuracy. Flow may be turbulent, or VTI measurement site may be difficult.
Despite limitations, Doppler echo is a cornerstone for non-invasive hemodynamic assessment. For more complex cases or when higher precision is required, methods discussed in advanced CO monitoring may be considered.
To understand how CO relates to overall body size, use our Cardiac Index Calculator. For comprehensive details on echocardiographic measurements, refer to guidelines from professional bodies like the European Association of Cardiovascular Imaging (EACVI) published resources.